Definition of Acne: Acne is a disease of the oil-producing glands and hair follicles of the skin. The most common areas affected are the face, neck, chest, back, shoulders and upper arms. The condition can have a devastating effect on emotional well-being. Scarring can occur with severe cases, worsened by the tendency of people to pick at and squeeze the lesions.
There are effective treatments. Most people wait to see a physician until the disease is advanced, causing physical and emotional distress. Early treatment is best, to avoid scarring and to limit the emotional toll of the lesions.
The American Academy of Dermatology classifies three levels of disease. With mild acne, there are few papules and pustules (pimples). Moderate acne has several to many pustules and papules, with few to several nodules. Severe acne is defined as many or extensive lesions, as well as many nodules.
Causes of Acne
Four factors working together cause acne:
- overproduction of oil
- shedding of dead skin cells, which plug hair follicles
- the bacterium Propionibacterium acnes,
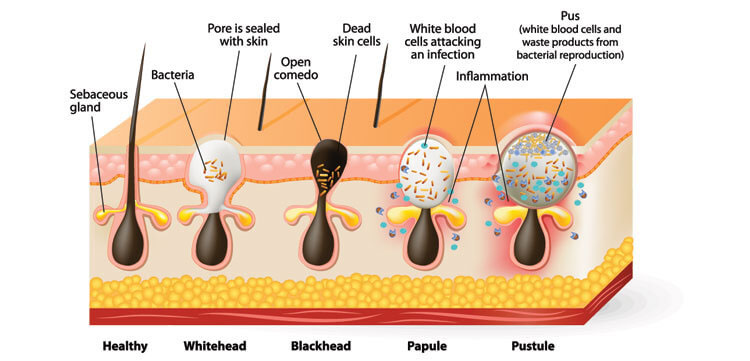
- inflammation – a response of the body’s immune system. A plugged hair follicle bulging above the skin is a whitehead. If the plugged follicle opens, the contents may darken, forming a blackhead. Blockage of follicles deep below the skin can cause cysts.
Contributing Factors
- Hormones, called androgens, increase in puberty, causing more sebum (oil) production. Certain oral contraceptives and pregnancy can also trigger more sebum production.
- Some medications worsen acne – corticosteroids, androgens and lithium.
- Some foods can trigger acne: dairy products and high-carbohydrate foods, such as bread and chips.
Greasy foods, chocolate, and dirty skin do not cause acne. Scrubbing the skin too vigorously and using harsh chemicals can worsen acne.
These risk factors can also trigger and aggravate acne:
- recurrent direct contact with greasy or oily substances, such as cosmetics
- family history of acne
- friction or recurrent pressure on the skin (cell phones, collars)
- stress – not a cause but a contributor
Signs and Symptoms of Acne
Acne occurs in several forms:
- Non-inflammatory lesions
- Comedones – whiteheads and blackheads
- Inflammatory lesions
• papules – small raised bumps from inflammation in hair follicles, flesh-colored or red and tender
• pustules – red spots with central, white pus
• nodules – large, solid, tender lumps below the skin’s surface – a buildup of sebum and dead skin cells deep in hair follicles
• cysts – painful, tender, lumps of pus beneath the skin’s surface, with the greatest risk for scarring
Acne Prevention
Even with a good response to treatment, or clearing entirely, oral and/or topical medication is continued to prevent new lesions. Other tips for acne prevention include:
- Wash acne-prone skin no more than twice daily, with gentle, oil-free products.
- Use an over-the-counter cream or gel, containing benzoyl peroxide and/or salicylic acid, to dry excess oil.
- Avoid heavy or oily cosmetics – use powders, rather than creams.
- Remove makeup before bed, to avoid clogging hair follicles.
- Wear loose-fitting clothing to avoid friction against the skin.
- Shower after sweating heavily – oil and sweat may trap dirt and bacteria on the skin.

Acne Treatment
There are effective acne treatments currently available, and new products are frequently introduced. They work in a variety of ways. Your dermatologist can guide your choice of products, refining treatment for your individual type and severity of disease. It may be several weeks before improvement is seen. Some treatments may make acne a little worse before it gets better.
Your dermatologist may recommend prescription medication, oral and/or topical. Follow your dermatologist’s instructions exactly. Failure to improve is most often caused by not using the medication exactly as instructed. Oral medication should not be used during pregnancy.
Types of treatment include:
- Over-the-counter topical treatments: these dry excess oil, kill bacteria, and remove dead skin cells. The active ingredient is usually benzoyl peroxide, salicylic acid, or sulfur. Side-effects are mild and usually transient, including skin irritation, dryness, flaking, and redness.
- Prescription topical treatments: adapalene, tretinoin and others, derived from vitamin A. They speed up production of skin cells, while shedding dead cells. There are also topical antibiotics which work by killing bacteria present on the skin. At times, a combination of treatments is used.
- Antibiotics: An oral antibiotic may be used short-term to reduce the number of bacteria in and on the skin. Many of the bacteria have become resistant to the antibiotics commonly used on skin. Side effects can be just unpleasant to dangerous – nausea, dizziness, skin discoloration and sun-intolerance. They can also decrease the effectiveness of oral contraceptives.
- Isotretinoin: This effective medication is usually reserved for moderate to severe cystic acne or acne that is resistant to other types of treatment. It is known to cause birth defects in women, and is therefore federally regulated to ensure lab testing monthly during the course of treatment. This applies to both women and men. Common side-effects include dry lips, mouth, nose and skin. Less common side effects include an increase in cholesterol, liver enzymes, and pancreatitis. It has also been linked with depression and suicide. Call your dermatologist immediately if you experience changes in mood or thoughts of harming yourself.
- Oral contraceptives: These usually contain a combination of estrogen and progesterone, which may improve acne in women. Side effects can include headaches, nausea, depression and breast tenderness. The most severe complications, and less likely, are an increased risk for heart disease, high blood pressure, and life-threatening blood clots, usually in the legs.
- Laser and light therapy: These treatments reach the deepest layers of the skin without harming the surface. They target acne-causing bacteria, may suppress oil production, and reduce inflammation. The skin improves in texture and this is often used for acne scarring.
- Other cosmetic procedures: Chemical peels and microdermabrasion can improve appearance by lessening discoloration and scarring, as well as reducing fine lines and sun damage. Side effects include redness, scaling, and less likely blistering or dyspigmentation.
Lifestyle and Home Remedies
- Wash problem areas with a gentle cleanser. Avoid masks, astringents, and facial scrubs; they can irritate the skin and make acne worse. Promptly remove sweat, dirt, and oils.
- Try over-the-counter lotions with benzoyl peroxide or salicylic acid, to remove excess oil and promote peeling.
- Avoid irritants, such as oily cosmetics, hair products, and even some acne concealers. Some products increase sun-sensitivity; use sunscreen that does not clog pores (non-comedogenic).
- Keep hair clean and off the face. Avoid touching or resting hands or objects against your face.
- Avoid tight clothing.
Alternative Medicine
It has been suggested that some dietary supplements may help treat acne, including:
- Tea tree oil: Gels containing 5 percent tea tree oil may be as effective as products containing 5 percent benzoyl peroxide. It may take longer to see improvement. It can cause an allergic reaction of the skin called contact dermatitis, and there is some evidence that it may cause breast development in young boys.
- Alpha-hydroxy acids: These are found in citrus fruits, sugar cane, apples, and grapes. When applied topically, these help remove dead skin cells and unclog pores. They may improve the appearance of acne scars. Adverse reactions to the acids include redness and irritation.
- Zinc supplements: These have a role in wound healing and reduce inflammation. Taking zinc with food may limit side effects, including a bad taste in the mouth, and nausea.
- Brewer’s yeast: A specific strain of Brewer’s yeast, “CBS 5926”, seems to help acne, but in some people it can provoke migraine headaches and gastrointestinal complaints.
Acne Scar Treatment
Acne scars can destroy self-confidence and quality of life can suffer. Your dermatologist is skilled in procedures which can decrease the visibility of scars, including:
- Soft tissue fillers. Collagen or fat from the patient’s body can be injected into areas of uneven texture. It fills out or stretches the skin, making the scars less visible. The results are temporary; usually periodic retreatments are necessary to maintain the effect.
- Chemical peels. Strong acid applied to the skin removes the surface layer and minimizes deeper scars. Skin type is important when choosing a chemical peel
- Microdermabrasion. This is a treatment in which tiny crystals are blown into the skin to polish the surface. Then, a vacuum tube removes the crystals from the skin. Skin irritation is minimal. Several treatments are needed.
- Laser, light sources and radiofrequency procedures. Laser therapy removes the surface layer of skin, and heats the deeper layer. New skin heals the wounds. Less intense lasers, pulsed light and radiofrequency devices don’t damage the skin surface, but heat the deeper layer, causing new skin formation. Recovery is quick, but the results are subtle, even after numerous treatments. Examples include the E-matrix and Infini. Both are very effective in treating active acne and helping the appearance of acne scars.
- Skin surgery. Plugs of scar tissue are removed from individual scars. Sutures (stitches), or a skin graft are used to close the defects left at plug sites.
See your dermatologist before severe disease develops and irreversible scarring occurs.
More information for the public
- Mayoral Dermatology: About Acne
- About.com: http://acne.about.com
- The American Academy of Family Physicians http://familydoctor.org/familydoctor/en/diseases-conditions/acne:html
References
- Feldman S, et al. Diagnosis and treatment of acne. Am Fam Physician. 2004 May 1;69(9):2123-2130
- National Institutes of Health: http://www.niams.nih/gov/health_info/acne/

